Combatting Superbugs: Innovations in the Fight Against Antibiotic Resistance
12/13/20244 min read
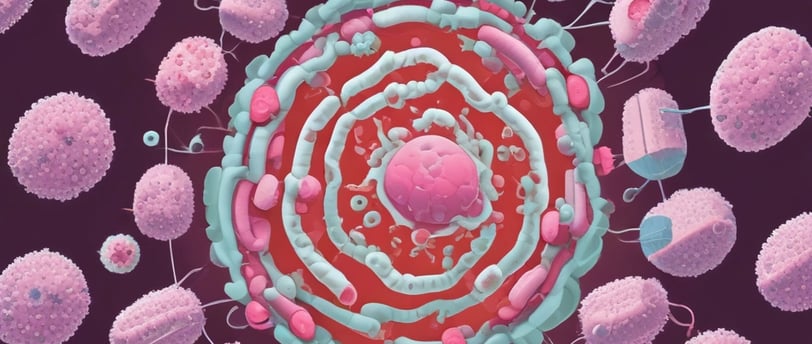

Understanding Antibiotic Resistance
Antibiotic resistance is a serious and growing public health concern that occurs when bacteria evolve in a way that reduces or eliminates the effectiveness of antimicrobial drugs. This phenomenon arises through various biological mechanisms, including genetic mutations and horizontal gene transfer, wherein resistant genes are shared between bacteria. When bacteria are exposed to antibiotics, those that possess resistance traits survive and replicate, leading to a population that is increasingly difficult to treat. As a result, infections caused by these resistant strains can become more severe and harder to manage.
Among the most notable resistant strains are the so-called "superbugs," which include well-known pathogens such as Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant Enterococcus (VRE), and multidrug-resistant Mycobacterium tuberculosis. These organisms have developed mechanisms to withstand multiple classes of antibiotics, making traditional treatments ineffective. The emergence of superbugs is often linked to factors such as overprescription of antibiotics, inappropriate use in agriculture, and inadequate infection control measures in healthcare settings. Each of these factors contributes to the accelerating problem of antibiotic resistance.
The implications of this trend extend beyond individual health; they pose a significant threat to public health systems worldwide. Infections that once were easily treated can now result in prolonged hospital stays, the necessity of more complex treatments, and, in severe cases, increased mortality rates. Furthermore, the economic burden associated with antibiotic resistance is substantial, driving up healthcare costs and impacting productivity. Addressing this urgent challenge is crucial to preserving the effectiveness of current antibiotics and ensuring the availability of effective treatments for future infections. As we explore innovative solutions to tackle antibiotic resistance, recognizing the underlying mechanisms and implications of this issue is imperative.
Innovative Approaches in Antibiotic Development
The emergence of antibiotic resistance presents a significant challenge in modern medicine, necessitating innovative approaches in antibiotic development. Traditional methods of developing antibiotics often result in a lengthy and costly process that is increasingly poorly aligned with the urgent need to combat resistant bacteria. To address these limitations, researchers are turning to cutting-edge technologies and methodologies that may enhance the discovery and efficacy of new antimicrobial agents.
One notable advancement in this field is the utilization of artificial intelligence (AI) to streamline drug discovery. Through sophisticated algorithms, AI can analyze vast amounts of data related to chemical compounds and their interactions with bacterial targets. This efficiency significantly accelerates the identification of promising candidates for new antibiotics. AI-driven models can also predict the potential effectiveness and safety of these compounds, thereby reducing the time and resources spent on ineffective drugs.
In addition to AI, phage therapy is gaining traction as an alternative to conventional antibiotics. This innovative approach utilizes bacteriophages—viruses that specifically target bacteria—to eliminate pathogens in a highly selective manner. Phage therapy has the advantage of adapting to bacterial mutations, allowing for a more versatile solution against evolving superbugs that traditional antibiotics cannot effectively manage.
Furthermore, the concept of combinatorial therapies is emerging as an effective strategy in the fight against antibiotic-resistant infections. By using a combination of different antimicrobial agents, researchers aim to enhance their overall effectiveness while minimizing the potential for resistance to develop. Such synergistic approaches can provide a multifaceted attack against superbugs, ensuring that bacteria are less likely to survive and adapt.
As antibiotic resistance becomes an increasingly pressing public health issue, the exploration of these innovative approaches in antibiotic development is critical. They represent a beacon of hope, offering the potential to create effective treatments that can outpace the capabilities of resistant bacteria.
Alternative Therapies and Preventative Strategies
As antibiotic resistance continues to pose a significant threat to public health, exploring alternative therapies and preventative strategies has become increasingly vital. One such innovative approach is the use of probiotics, which are live microorganisms offering health benefits, particularly in maintaining gut health and enhancing the immune response. Probiotics can help inhibit the growth of harmful bacteria, thus reducing the reliance on antibiotics to treat infections. Their role in modulating the gut microbiome is critical in preventing the onset of infections, particularly in individuals at risk of antibiotic-induced dysbiosis.
Another promising avenue is the development and use of vaccines. Vaccines serve as a preventive measure by inducing immunity against specific pathogens, effectively decreasing the incidence of infections that may otherwise require antibiotic treatment. Innovations in vaccine technology, including mRNA vaccines, have demonstrated potential for rapid development in response to emerging infectious diseases, helping ensure public health while reducing the need for antibiotics.
Immunotherapy also presents a shift in treatment paradigms. This approach leverages the body’s immune system to target and eradicate infections. By focusing on enhancing the host's immune response, immunotherapy may significantly reduce antibiotic usage and combat antibiotic resistance. Coupled with emerging non-antibiotic antimicrobials, such as bacteriophages and antimicrobial peptides, these methods expand the toolbox for fighting bacterial infections without contributing to resistance.
Moreover, effective hygiene practices and rigorous infection control measures are paramount in both healthcare facilities and community settings. These practices include proper handwashing, sanitation, and disinfection protocols, which significantly mitigate the spread of resistant bacteria. Educating the public on the importance of hygiene can help cultivate a culture of prevention, thereby limiting the reliance on antibiotics and ultimately preserving their efficacy for future generations.
Global Collaboration and Policy Initiatives
Tackling antibiotic resistance necessitates a concerted global effort, as superbugs do not recognize national boundaries. The World Health Organization (WHO) has been at the forefront of international initiatives aimed at combating antibiotic resistance. One of its landmark actions includes the Global Action Plan on Antimicrobial Resistance, which emphasizes the need for countries to develop national action plans tailored to their specific contexts. Such cross-border initiatives have proven critical in facilitating knowledge sharing, standardizing policies, and fostering cooperation among nations to reduce the overuse and misuse of antibiotics.
Policy changes play a vital role in regulating antibiotic use effectively. Governments worldwide are urged to implement strict policies that promote responsible prescription practices. These policies can include limiting the sale of antibiotics without a prescription and developing guidelines to curb unnecessary usage in both human health and agriculture. By aligning healthcare regulations with international standards, countries can significantly mitigate the rise of antibiotic-resistant pathogens.
Moreover, education serves as a powerful tool for promoting responsible antibiotic consumption among the public and healthcare professionals. Awareness campaigns aimed at educating communities on the dangers of antibiotic misuse can substantially influence individual behavior. Knowledge empowers patients to engage in discussions about antibiotic prescriptions with their healthcare providers, advocating for judicious use. Likewise, training programs for healthcare professionals are vital in ensuring they are up-to-date with the latest guidelines on antibiotic stewardship.
Successful case studies from various countries illustrate the positive impact of well-executed collaborations and policies. For instance, Sweden has implemented a comprehensive national strategy to reduce antibiotic use which has led to a significant decline in prescriptions. Such examples serve as benchmarks for other nations to follow. Strengthening alliances among individuals, healthcare providers, and governments is essential for establishing a formidable front against the looming threat of antibiotic resistance.
Discover
Explore science, life, and hands-on experiments.
Engage
Learn
contact@exploreexplain.com
+1234567890
© 2024. All rights reserved.
